Our Pipeline
At MBX, we are reimagining how patients live with endocrine and metabolic diseases.
Enabled by our proprietary PEPTM platform technology, we have a growing pipeline of therapeutic candidates in various stages of clinical development.
“Our pipeline of PEP candidates includes clinically validated targets with well-defined regulatory pathways to address significant unmet medical needs. Our efforts will make a meaningful impact in improving the lives of individuals with endocrine disorders.”
Development Programs
MBX 2109 is an investigational new drug (delivered via sub-cutaneous injection), that is designed as a potential long-acting hormone replacement therapy for the treatment of chronic hypoparathyroidism, or HP. Leveraging our proprietary PEP platform, we designed MBX 2109 to treat the underlying pathophysiology of HP by providing a continuous, infusion-like exposure to parathyroid hormone, or PTH, with convenient once-weekly administration.
In Phase 1 clinical trials*, MBX 2109 was generally well-tolerated with no drug-related severe or serious adverse effects. Our Phase 2 trial, called Avail™, is currently recruiting patients. More information about the Avail trial can be found here.
We are also conducting a clinical trial of MBX 2109 in adults with normal and impaired renal function. Information about this study can be found here.
Hypoparathyroidism Background
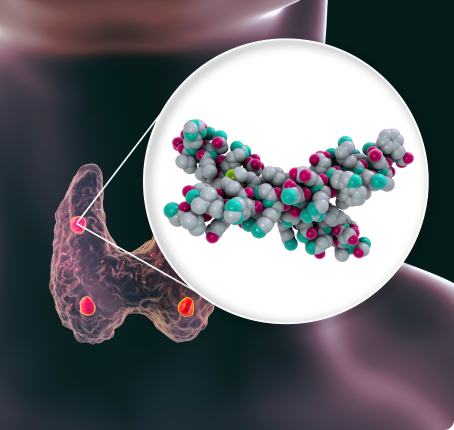
Parathyroid hormone is a peptide hormone secreted by the parathyroid glands that regulates calcium and phosphate levels in the blood through its effects on bone, kidneys and intestines. The parathyroid glands are located behind the thyroid gland in the neck.
Hypoparathyroidism is a rare condition in which the parathyroid glands fail to produce sufficient amounts of PTH. It affects more than 260,000 persons throughout the United States, Europe and Japan.1-3 HP is often caused by damage to or removal of the parathyroid glands during surgery for another condition but it can be caused by an autoimmune process or other etiologies. Insufficient PTH results in a lowering of blood calcium levels (hypocalcemia) and an increase in phosphate levels (hyperphosphatemia).
Hypocalcemia can cause a variety of symptoms ranging in intensity from mild to severe, including muscle cramps and spasms in the hands and feet and numbness or tingling around the mouth and fingers and toes.4 Depression, confusion and loss of memory have been reported5 and certain individuals may develop calcium deposits in the brain or the kidneys, which can lead to impairment of kidney function.4,6,7 Persons with HP may also be more prone to developing kidney stones.4,7 Less often, more serious complications can occur including seizures or cardiac arrhythmias (abnormal heartbeat).7,8 Consequently, HP can greatly impact a person’s quality of life, interfere with their daily lives, and negatively impact their ability to work.9
Treatment of HP is aimed at raising calcium levels in the blood to provide relief of symptoms without causing abnormally high levels of calcium in the blood (hypercalcemia) or urine (hypercalciuria). The mainstay of treatment is calcium supplements and active vitamin D. Long-term use of these can contribute to the development of calcium deposits and kidney stones.
* The results observed from preclinical studies or early-stage clinical trials of our product candidates may not necessarily be predictive of the results of later-stage clinical trials that we may conduct. Similarly, positive results from such preclinical studies or early-stage clinical trials may not be replicated in our subsequent preclinical studies or clinical trials.
MBX 1416 is an investigational therapy in development as a potential treatment for post-bariatric hypoglycemia (PBH). We aim to prevent the occurrence of severe hypoglycemia (very low blood sugar) in individuals with PBH so they can lead healthier lives. MBX 1416 is currently in Phase 1 clinical studies. More information can be found here.
Post-bariatric hypoglycemia (PBH; low blood sugar) is rare but increasingly recognized complication of bariatric surgery, occurring after both Roux-en-Y gastric bypass and vertical sleeve gastrectomy. Most patients present within 1 to 4 years of surgery.1
Hypoglycemia (low blood glucose) can occur 1-3 hours after ingestion of a carbohydrate-rich meal. In some individuals, neuroglycopenic symptoms may develop, which can include confusion, weakness, dizziness, blurred vision and loss of consciousness or seizure. These symptoms can result in trauma to the individual. Often individuals experiencing neuroglycopenic symptoms are refractory to conservative therapy with dietary changes. Medications such as acarbose, diazoxide or octreotide may be used off-label by doctors, but poor tolerability limits their use, and none are approved to treat PBH. There remains a significant unmet need to develop therapies to address this condition.

Obesity is a common condition in the United States, with more than 2 in 5 adults 20 and older (42.5%)1 being afflicted. A chronic condition, it can be caused by a variety of factors including, but not limited to, eating high-calorie, low nutrient foods and beverages, lack of physical activity, some medications, and genetics.
Screening for obesity is performed by healthcare providers using body mass index (BMI), which measures the percent of body fat in an individual. A person whose weight is higher than what is considered to be a normal weight for a given height is described as being overweight or having obesity.2 In the case of adults 20 and older, a BMI >30 is classified as obese and >40 is severely obese.
A high percentage of body fat can put an individual’s health at risk as it increases the likelihood for developing more than 200 health problems such as high blood pressure, type 2 diabetes, depression, cancer and heart disease – the leading cause of death in the United States. In fact, research shows that there has been a three-fold increase in obesity-related deaths from heart disease in the United States between 1999-2020.3
The biomedical, psychosocial, and economic consequences of obesity have substantial implications for the health and well-being of the U.S. population.4 There is also a bias to be addressed, as it is well documented that those who feel stigmatized by obesity can suffer extreme emotional distress and be subject to discrimination, which can lead to further negative health impacts, including depression and additional weight gain.5
While lifestyle changes may influence weight loss and reductions in BMI, obesity is a complex problem that often does not have a single solution. Whether behavioral, pharmacologic, or surgical, this epidemic may benefit from a holistic multifaceted approach.6
Our world-class technology platform was developed with the flexibility to tackle a variety of diseases that could benefit from more precise therapeutic options. We have an active research and design program, through which we have identified numerous additional candidates in both rare and prevalent diseases. These candidates are in various stages of pre-clinical development.
From Pipeline to Promise
World-Class Peptide Platform
Explore what patients have to say and learn more about current clinical trials and how MBX Biosciences is striving to make a difference for people living with hypoparathyroidism, post-bariatric hypoglycemia and obesity.
Patients